
What Is the Best
Yeast Infection
Treatment?
Published on October 19, 2020
Updated on June 11, 2025
Written by Kathleen Morrison
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
If you’re tired of the itching and need to know what actually works for a yeast infection, the short answer is: an oral antifungal medication like prescription fluconazole is often the go-to for fast, effective relief.
But here’s the thing—what works best can really depend on you. Your body, your symptoms, your lifestyle, and even how often yeast infections show up for you can all shape which treatment is the right fit.
There’s no one-size-fits-all fix for vaginal yeast infections (or vaginal Candidiasis), and that’s okay. From oral meds to creams, suppositories, and supportive care, there are options out there—and this guide will help you feel confident exploring them.
Let’s talk about what’s available, what to consider, and how to choose a treatment that actually makes sense for your body and life.
Wisp treatment options are available only after consultation with a licensed medical professional. You should consult with your healthcare provider before starting a new supplement or treatment regimen. Individual results may vary.
The best treatments for fast relief
When that itch, burn, or irritation shows up, you want to feel better, like, yesterday. Luckily, there are some solid options that can help you get quick relief and get back to feeling like yourself.
A typical go-to is antifungal over-the-counter (OTC) vaginal creams or suppositories. These contain ingredients like miconazole or clotrimazole that work directly where it hurts to calm things down. They’re easy to grab and simple to use, and they can do the trick for many people with a mild yeast infection.
If you go the OTC route, it’s key to stick with the instructions—usually using the cream or suppository for about three to seven days, depending on how things look and feel. Sometimes you might notice a little burning or irritation at first, but that usually fades as the medicine gets to work.
If the OTC options don’t quite cut it, or if vaginal infections are popping up more than you’d like, it’s time to chat with a healthcare provider. They might suggest a prescription medicine like fluconazole—an oral antifungal taken as a single dose that works throughout your body to tackle the infection.
For tougher cases, prescription creams or suppositories like terconazole can be a game-changer. These usually need a longer course (think seven to fourteen days) to make sure the infection gets the full send-off.
The best treatments for recurrent Yeast Infections
If you’re finding yourself facing yeast infections over and over—like four or more times a year—it can be super frustrating and honestly a little exhausting. When infections keep coming back, it usually means it’s time to try a different game plan.
One way to tackle this is with a maintenance treatment. This means using antifungal meds, either by mouth or vaginally, on a regular schedule (usually once a week for a few months).
The idea? To help keep things balanced and stop those annoying repeat infections from sneaking back in.
Long-term changes
Besides medication, some simple lifestyle tweaks might make a difference, like:
- Choosing breathable cotton underwear
- Changing out of wet or sweaty clothes quickly
- Steering clear of super-tight pants or leggings
- Cutting back on sugar and refined carbs
- Adding probiotics to support your good bacteria
If you have a health condition like diabetes or HIV that affects your immune system, yeast infections might show up more often. In that case, teaming up with your healthcare provider to manage your overall health is key.
The best treatments during pregnancy
Pregnancy brings all sorts of changes, and yeast infections are pretty common thanks to those shifting hormones.
The tricky part? Not every treatment out there is safe for you and your little one during this special time.
If you think you’ve got a yeast infection while pregnant, the best move is to check in with your healthcare provider first. They’ll help confirm what’s going on and guide you toward options that are gentle and safe for both of you.
Wisp does not provide treatment to pregnant patients.
Your choices during pregnancy
Here’s the lowdown on what’s usually considered safe when you’re expecting:
- Topical antifungals like clotrimazole or miconazole are the most common go-tos during pregnancy.
- These come as creams or suppositories.
- They work right at the source to calm down the yeast and soothe symptoms of a yeast infection.
- Generally considered safe and effective, especially when used as directed.
- Oral fluconazole (aka Diflucan) is typically not recommended during pregnancy, especially in the first trimester.
- Some studies have linked it to risks when taken in high doses or early on.
- That said, in certain cases, your provider might still prescribe a single low dose if the infection is severe or doesn’t respond to topical treatments.
- If you're considering this route, it’s definitely a conversation to have with your doctor.
When you're pregnant, it's always a good idea to check in with a provider before starting any treatment, even OTC options. Your body’s doing a lot right now, and you deserve care that meets you right where you are.
Tips for your treatment
When you do use any treatment, follow the instructions carefully—don’t go overboard. Most yeast infections clear up after a few days, so if symptoms like vaginal discharge or itching get worse, reach out to your healthcare provider for advice.
Also, keeping things clean and comfy down there can help you feel better and keep irritation at a minimum, so you can cope. Wearing breathable underwear, avoiding scented products or douching, and gently drying the area can make a big difference.
The best treatments for men
Yep, men can get yeast infections, too—though it’s less talked about. If you notice redness, itching, a rash on your penis, or burning when you pee or during sex, it could be a yeast infection. Totally normal, but definitely something you want to handle.
Treating yeast infections for men is pretty similar to how it’s done for women, with a few tweaks. Over-the-counter antifungal creams like clotrimazole or miconazole can be applied right to the spot that’s acting up.
What’s different for dudes?
Sometimes, if the infection is a stubborn one or keeps coming back, your healthcare provider might suggest an oral antifungal like fluconazole (Diflucan).
Just a heads-up: the dose and how long you take it can be a bit different from what women typically get.
Good hygiene is key, especially if you’re uncircumcised. Make sure to clean gently but thoroughly, dry the area well after showers or swimming, and avoid tight clothes that can trap moisture and make things worse.
When should you see a doctor?
If this is your first time dealing with symptoms, it’s smart to check in with a healthcare provider to get a clear diagnosis. Some other things, like certain sexually transmitted infections (STIs) or bacterial infections, can cause similar symptoms but need different treatments.
Also, if you find yourself facing repeat yeast infections or your symptoms don’t clear up after trying over-the-counter stuff, don’t wait—see a healthcare provider. They can figure out if something else is going on, like an immune issue or something like diabetes that needs attention, and help you find the right treatment.
Can men pass a yeast infection to their female partner?
Yep, it happens—and it's more common than people think. If you’ve got a penis and you’re dealing with a yeast infection (especially if you’re uncircumcised), it’s totally possible to pass it to a partner during sex. Yeast can hang out under the foreskin or on the surface of the skin, even if symptoms aren’t obvious yet.
Don’t worry, you’re not in trouble. But if one partner gets treated but the other doesn’t, the infection can bounce back and forth like an unwanted ping-pong game. So, if you or your partner has symptoms, it’s smart for both of you to treat at the same time.
The best treatments for children and teens
Yeast infections can pop up in kids and teens, too, though it’s less common than in adults. You might notice redness, itching, or discharge around their private parts (or their mouth). Totally normal, but definitely worth sorting out.
How you treat it depends on their age and how things look.
Wisp products and services are for adults 18 and over, and Wisp does not provide treatment to minors under the age of 18.
Little ones
For babies and toddlers, a gentle clean with warm water and mild soap usually does the trick, followed by a little antifungal cream if the doctor says it’s needed.
Older kids and teens
For bigger kids and teens, over-the-counter antifungal creams or suppositories might be the way to go, but always check in with your pediatrician or healthcare provider first. They’ll make sure the treatment is safe and just right for their age and size.
Sometimes, a prescription might be needed. Doctors can prescribe oral medication like fluconazole (Diflucan) if that’s the best move, with doses carefully matched to weight and how serious the infection is.
Tips for parents and caregivers
If you think your child might have a yeast infection, the best first step is a visit to the healthcare provider to confirm what’s going on. Sometimes, other things like bacterial infections or irritation from diapers or soaps can cause similar symptoms, so it’s good to get a clear answer.
Keeping things clean and dry is another important step—changing diapers often, using gentle soap and warm water, and skipping anything with strong scents or harsh chemicals like bubble baths or lotions that might irritate.
For teens, chatting openly about good hygiene and what to watch out for can make a huge difference. Encouraging breathable cotton underwear and changing out of sweaty or wet clothes quickly helps keep things comfy and happy down there.
What about at-home options?
Thinking about trying natural or at-home options before jumping into prescription medications? Totally get it—many people want to start with gentle, easy options that feel more “you.” While science hasn’t fully given all of these the green light, some folks find they sometimes help care for your body and bring back some comfort.
Here’s a breakdown of natural and at-home options you might know about:
Natural aids you’ve probably heard of
There are a few common ones you’ll know about:
- Coconut oil: Known for its antifungal properties, it can be gently applied to the affected area. It could bring some relief if you’re feeling serious irritation.
- Tea tree oil: Has antifungal and antiseptic qualities but needs to be diluted with a carrier oil like coconut or olive oil before applying to avoid irritation.
- Probiotics: Found in supplements or fermented foods like yogurt and kefir, probiotics (especially strains like Lactobacillus acidophilus) may help keep your natural bacteria balanced.
- Boric acid suppositories: Sometimes recommended for infections that just won’t quit. But heads up—boric acid can be toxic if not used exactly as directed, so following the instructions is really important.
A friendly reality check
While natural options sound nice and cozy, it’s smart to be careful. Some of these can irritate your skin or cause allergic reactions, especially if used straight-up or too much.
Also, natural options are never as strong or fast-working as the usual treatments, especially if your infection is a stubborn one or keeps coming back. If things don’t get better with natural approaches, it’s a good idea to check in with a healthcare provider who can help figure out the next best steps.
If you’re pregnant, have a health condition that causes a weakened immune system, or are taking medications, definitely chat with your healthcare provider before trying any natural solutions. Some natural products can interact with meds or have effects you wouldn’t expect.
When to start at home and when to see a pro
If you’re healthy and your symptoms are mild, at-home options could be a good starting point to take the best possible care of your vaginal health. However, getting the real deal (i.e., meds) is almost always your best bet when you’re dealing with an infection.
If you’re pregnant, have a weaker immune system, or your symptoms feel severe or keep popping back up, it’s extra smart (and important) to get professional advice. A healthcare provider can help make sure you’re treating the right issue safely and effectively.
And if you’re ever unsure whether what you’re experiencing is actually a yeast infection (sometimes symptoms overlap with other conditions like bacterial vaginosis or trichomoniasis), checking in with a pro can save you time and frustration.
Taking charge of Yeast Infections
Yeast infections are super common and, yeah, they can be a total pain. But the good news? There are plenty of ways to tackle them—from easy over-the-counter options to prescription treatments—so you don’t have to just grin and bear it.
Choosing the right treatment for you comes down to what feels best for your body, how strong your symptoms are, and your own preferences. Everyone’s different, and that’s okay.
Ready to take control and say goodbye to discomfort? Check out Wisp’s yeast infection treatments and get started on your path to feeling amazing again—no judgment, just real talk and real care.
Frequently Asked Questions (FAQ):
What gets rid of a yeast infection the fastest?
If you’re all about quick relief, over-the-counter antifungal creams or suppositories (like clotrimazole or miconazole) can start working fast. Prefer to keep things simple? A one-time oral antifungal tablet like fluconazole (aka Diflucan) is a super-effective option for many people. You’ve got choices.
Which yeast infection medicine is most effective?
Oral fluconazole is often the go-to for a reason. It works from the inside out and can be especially helpful if your yeast infection feels a little more intense or just keeps coming back. But the “best” option depends on your body, your preferences, and how your symptoms are showing up.
Does Monistat 1 or 3 work better?
Both get the job done, but they work a little differently. Monistat 1 is a one dose wonder, which can be super convenient. Monistat 3 spreads treatment over three days and can be a gentler option if your body tends to be sensitive to stronger meds.
Which is better, Monistat or Vagisil?
Here’s the lowdown: Monistat actually treats the yeast infection. Vagisil, on the other hand, helps with itch and discomfort, but it doesn’t clear the infection itself. If you’re looking to knock out the root cause, Monistat’s your better bet.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.

Diflucan, Generic Fluconazole (Yeast Antifungals)
Starting at $45.00
Prescription antifungals used to treat vaginal yeast infections
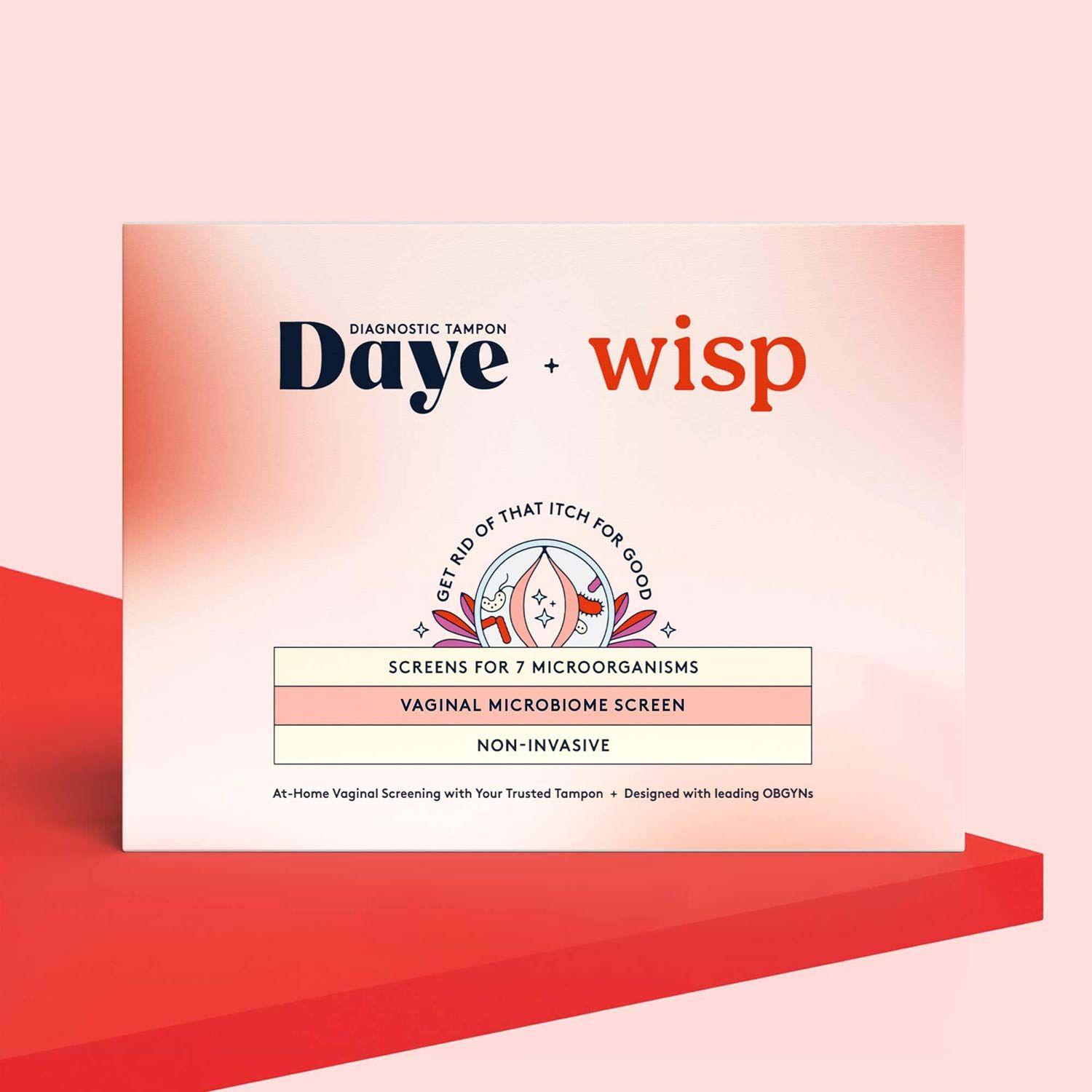
At-Home Vaginal Microbiome Screen by Daye
$125.00
Understand your vaginal microbiome balance and risk of infections using a non-invasive at-home tampon collection kit.


