Written by Kathleen Morrison
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
Key takeaways
- Migraines with aura give your body an early heads-up with visual, sensory, or speech changes that usually appear 10 to 60 minutes before the headache starts.
- Visual auras are the most common, but tingling, numbness, difficulty speaking, and balance issues can also signal an oncoming migraine.
- Auras happen because of shifts in brain electrical activity, changes in nerve function, genetics, and triggers like hormones, stress, sleep, and certain foods.
- Knowing your personal triggers and having a plan—whether that’s medications, calming techniques, or hormone-friendly birth control—can help give you a sense of control over your migraines.
Menopause Migraines Decoded
So, you’ve made it to menopause—and surprise, your head decided to join the chaos. But this isn't uncommon: loads of women notice their migraine patterns change during menopause, and those shifts can feel unpredictable, intense, and just plain unfair.
The reason? Hormones (of course). As your estrogen levels fluctuate and then dip during perimenopause and menopause, your brain’s pain pathways and blood vessels react, sometimes in ways that trigger new or more frequent migraines. You might find that the headaches you used to get around your period feel different now, or if you’ve never had migraines before, suddenly you’re getting to know them all too well.
Once you know that menopause migraines are often hormone-related, you can start taking charge, whether that’s exploring treatment options, making simple lifestyle tweaks, or scheduling an online migraine consult to help you figure things out.
What does a menopause migraine feel like?
Menopause migraines come with their own flair, and not in a fun way. They can hit hard, often starting with that deep, throbbing pain on one side of your head that makes even the idea of movement sound unbearable.
You might notice the pain pulsing or pounding, light and noise feeling like personal attacks, and a desperate need for a quiet, dark room. Nausea is super common too (and yep, sometimes vomiting comes along with it). Temperature swings are also part of the mix... You might feel unusually hot or freezing, thanks to the delightful combo of migraines meeting hot flashes, and night sweats.
Menstrual migraines often run on a schedule with your menstrual cycle, but menopause migraines can be wildcards. They can last anywhere from a few hours to a few days, and sometimes come with a warning sign called an aura: think flashing lights or zigzag patterns before the pain sets in. You might also notice some other new, unique migraine symptoms you hadn't experienced before. Fun.
Why does menopause make headaches worse?
Basically, hormonal fluctuations can make your brain’s pain signals go a little haywire. During your reproductive years, estrogen follows a steady rhythm, rising and falling with your cycle. But with the menopause transition, that rhythm disappears, and your body starts deciding on a whole new normal for you.
The estrogen drop
Estrogen and migraines are kind of frenemies. When estrogen levels drop suddenly (as they often do in perimenopause), your brain doesn’t love it. These quick dips can mess with your pain pathways, especially the trigeminal nerve, which plays a big role in facial sensation and headache pain.
The American Migraine Foundation has shown that lower estrogen levels also affect serotonin, the feel-good chemical that can help regulate pain. When both take a nosedive, your body becomes more sensitive to migraine triggers. That’s also why people who go through surgical menopause (rather than natural menopause) sometimes notice a heavier migraine burden than before.
Blood flow
Here’s another twist: estrogen usually helps your blood vessels stay relaxed and flexible. When levels decline, those vessels can become a bit stiffer and more reactive, which means everyday triggers (like stress or salty snacks) might hit harder. This can set off inflammation and pain that lead to migraine pain.
Hot flashes play a role, too. The same vascular changes behind those fiery waves are linked to migraine activity. If you’re dealing with frequent migraine headaches and intense hot flashes, it’s worth checking in with your doctor, not just for comfort, but to look out for any cardiovascular disease risk.
How are hot flashes and headaches connected?
During menopause, you might notice sudden waves of heat starting in your chest, spreading up your neck, and leaving you flushed and sweaty. That’s your blood vessels opening up (super fast!) to release heat, and we call these "vasomotor symptoms."
But here’s the catch: that same kind of blood vessel activity can also trigger migraine attacks. Women who get frequent hot flashes are usually no strangers to experiencing migraines, too. It’s not just the heat; you might also notice that an intense hot flash can hit right before a migraine kicks in. And if night sweats are waking you up, that lost sleep can make your mornings feel extra rough. When your sleep cycle gets messy, your migraine threshold drops, making headaches more likely to pop up.
It all ties back to the hypothalamus, the part of your brain that helps control body temperature and—surprise—also plays a role in migraine activity. Basically, your brain is multitasking, and sometimes it just needs a little extra support.
How to track your migraine pattern
Keep tabs on your menopause migraines with a simple diary or an app like MigraineBuddy. Focus on these key things:
- Record each attack: Note the time, duration, location, pain intensity, and any extra symptoms.
- Track other menopausal symptoms: Include hot flashes, night sweats, mood swings, or vaginal dryness.
- Follow your cycle: If you’re still having menstrual periods, mark them down. Hormone fluctuations can create patterns.
- Log medications and supplements: Jot down what you take, how quickly it works, and how it compares to over-the-counter options like Excedrin Migraine or Advil.
- Stick with it: Commit to tracking for at least three months to spot trends and get more control over your migraines.
MigraineBuddy and Wisp Inc. are separate and non-affiliated companies.
Migraine treatment options
These days, medical options give you a bunch of ways to get a handle on your migraines. Menopause changes the game, so healthcare providers take a look at your overall symptoms, heart health, and any hormone therapy you might be using.
You can also book a migraine consultation online, making it easy to get a personalized treatment plan delivered right to you without leaving home.
Preventive migraine treatments
If you’re having more than four migraine attacks a month, preventive medications can be a game-changer:
- Traditional options include beta-blockers, antidepressants, and anti-seizure meds
- Newer options like CGRP inhibitors (Aimovig, Ajovy, Emgality) target migraine pathways directly
You can also complement meds with natural approaches:
- Magnesium (400–600mg daily) can help keep your blood vessels chill
- Riboflavin (400mg daily) and Coenzyme Q10 (300mg daily) can help with migraine frequency
Acute relief
Even with preventive strategies, sometimes you need fast relief:
- Over-the-counter options like Aleve or Tylenol Extra Strength can help tackle mild attacks if you catch them early
- Prescription triptans are the go-to for moderate to severe migraines
- Newer options like Ubrelvy and Nurtec ODT offer relief without affecting blood vessels—great if heart health is a concern
Hormone replacement therapy
Hormone replacement therapy (HRT) can help make a real difference for some women. Steady hormone levels through patches like Climara, Vivelle-Dot, Minivelle, Dotti, or gels like EstroGel and Divigel can help manage fluctuations from triggering migraines.
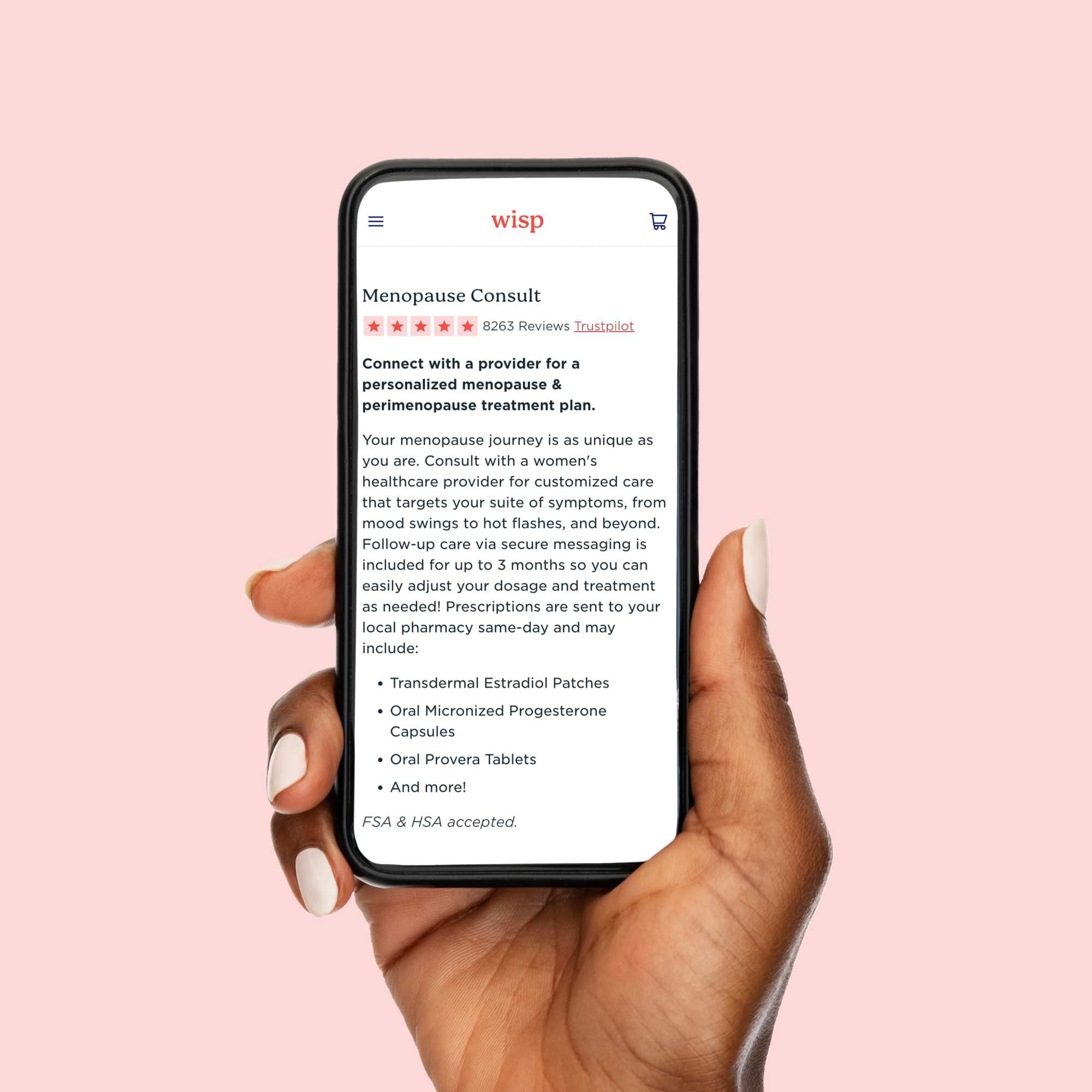
But HRT isn’t a one-size-fits-all. Women with migraine aura need to be careful because certain HRT types increase stroke risk. For personalized guidance, an online menopause consult can help you chat with specialists and get a treatment plan that works for you.
Lifestyle shifts
Alongside your prescribed migraine care, making some simple lifestyle tweaks can give your head a break and help make attacks more manageable.
- Sleep like it’s sacred: Consistent sleep schedules and a cool, dark room can help limit night sweats from disrupting your rest and keep your migraine patterns steadier.
- Eat and hydrate with intention: Balanced meals and steady hydration keep blood sugar even, which can help make a difference in how you feel. Pay attention to any foods that might make you feel worse—think aged cheeses, processed meats, or artificial sweeteners. They’re different for everyone. Certain dietary supplements can also complement your routine if you check in with a provider first.
- Move in a way that feels good: Regular moderate exercise, like walking or swimming for about 30 minutes most days, can help with frequency. Gentle movement practices like yoga or tai chi double as stress relief while improving flexibility. Skip the high-intensity stuff if a migraine is active.
These lifestyle steps aren’t a replacement for your prescribed care—they work alongside it, giving you more tools to manage menopause migraines and feel more in control.
When to talk with your doctor
If you notice sudden, severe headaches that feel different from your usual pattern, or headaches accompanied by fever, a stiff neck, confusion, or changes in vision, reach out to a healthcare provider right away. It’s also a good idea to check in if your migraines are becoming more frequent or intense, if over-the-counter options aren’t cutting it, or if headaches are interfering with your daily life more than a couple of times a month.
Be sure to share all of your menopause symptoms, not just your headaches. Hot flashes, sleep changes, and other symptoms all play a role in figuring out the best approach for you. Don’t settle for thinking migraines are “just part of menopause.” The right treatment combo can make a huge difference, helping you feel more like yourself again.
Take charge of your menopause migraines
Menopause migraines can feel like an unexpected plot twist in an already complex chapter of life, but understanding how hormonal changes play into your headaches gives you the upper hand. Keeping track of patterns, trying lifestyle tweaks, and teaming up with knowledgeable providers can help you build a game plan that actually works.
From preventive medications and quick-relief options to thoughtful hormone therapy, there are plenty of ways to tackle these headaches. You don’t have to face them alone—specialized telehealth services make it easy to get a personalized menopause migraine consult from the comfort of your home.
Ready to feel like yourself again? Book your migraine consult with Wisp today and get the care tailored to you.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.