Written by Kathleen Morrison with Hormonally
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
Menopause can bring a lot of uncomfortable changes to your body, and one of them might be noticing more bladder discomfort or frequent urinary tract infections (UTIs). This obviously isn’t fun, but it’s totally normal. It’s just your body adjusting to a shift in hormone levels.
Luckily, with a bit of knowledge and some thoughtful lifestyle choices, many people find ways to feel more comfortable and keep those annoying infections at bay. Taking the time to understand what’s happening and what might be triggering these changes can help you feel more in control, and remember, you don’t have to face it alone.
Connection between Menopause and UTIs
Menopause brings some major changes to your body, and one of the things that can pop up more frequently is UTIs. Hormonal shifts (particularly a drop in estrogen) can affect the urinary tract, making it easier for infections to take hold. Here’s how menopause and UTIs are connected and what you can do to feel more in control.
Hormonal Changes
As estrogen levels dip during menopause, the protective layers of the urinary tract can become thinner and less elastic, making it easier for that bad bacteria to get where it’s not wanted. This change can make people more prone to UTIs, but you don’t have to navigate it alone.
Some people talk with their healthcare provider about options like topical estrogen treatments to help rebuild the tissue and support bladder health. It's a good way to strengthen those natural barriers.
Why UTIs are More Common During Menopause
The drop in estrogen doesn’t just affect the tissues; it also changes the balance of bacteria in the vaginal area. With this shift, harmful bacteria can thrive, increasing the chances of developing a UTI.
But there are simple things you can do to help keep things balanced, like wearing breathable fabrics or using water-based lubricants when you get intimate to reduce friction. These small habits can help make a big difference in your urinary health.
The Role of Estrogen in Urinary Health
As you may have realized, estrogen plays a major role in maintaining the strength and structure of tissues in the urinary tract. When estrogen decreases, the tissues can become more vulnerable, leading to micro-tears or bacterial entry.
For many, estrogen therapies, like low-dose topical treatments, can help rebuild tissue thickness and restore the natural balance. Your healthcare provider can help find the right approach based on your unique needs and medical history.
Symptoms of UTIs in Menopausal Women
It’s important to note that UTIs can show up a little differently during (and post) menopause—sometimes they’re subtler or feel more like general discomfort. The good news is that being able to recognize these shifts early means faster relief and can help keep infections from getting worse.
But here's the thing: menopause symptoms can sometimes hide UTI signs. For example, because of menopause, you might experience:
- Back pain or fatigue that doesn't go away with rest
- Changes in your bladder habits, like feeling like you need to go more often in general
- Discomfort that seems more like general aches than the typical UTI burning
These things can easily be written off as just part of menopause, but keeping an eye on them and reaching out to a healthcare provider when something feels off is important. A quick check can make sure everything’s on track and help you feel more in control of your body.
We get it—life is busy, and it’s easy to let little changes slide. But by staying aware and listening to your body, you can catch things early before they turn into bigger problems. Early action means less stress later!
Common UTI Symptoms
Here are the typical urinary symptoms that you may be familiar with:
- Burning or stinging while peeing
- Frequent urination or the sudden urge to go
- Cloudy or foul-smelling urine
- Blood in your urine, which might look pinkish
- Low abdominal pain or discomfort
If you notice any of these signs, it’s a good idea to check in with your healthcare provider. A simple urine test can confirm whether it's a UTI and get you on the right track for treatment.
Less Typical UTI Symptoms During Menopause
Sometimes, UTIs don’t show up in the usual ways. During menopause, you might experience:
- A dull ache in your back or sides
- Unexplained fatigue that doesn’t go away with rest
- Mood swings or unexpected bladder spasms
These symptoms might feel like just part of the menopause journey, but they could also be signs of a UTI. It's helpful to notice if any of these issues pop up after certain activities or at specific times. Tracking these details can be really useful when talking to your healthcare provider.
Catching things early means you can get the right treatment and avoid more serious issues down the line, like a kidney infection. The sooner you reach out for help, the sooner you can feel better.
Taking Care of Your Urinary Health During Menopause
When it comes to urinary health during menopause, small, everyday habits can make a big difference in how you feel. For some, a few simple lifestyle changes are all it takes to stay comfortable. For others who experience recurring UTIs, a more tailored approach might be necessary. Whatever your situation, being proactive and taking charge of your health can make a world of difference.
Lifestyle Changes
A few small changes to your daily routine can really go a long way in supporting your urinary health. Here are some easy habits to try:
- Wear breathable underwear: Cotton or other natural materials help keep things dry and comfortable, which can make a huge difference.
- Stay hydrated: Drink water throughout the day. Not only does it keep you feeling good, but it also helps keep your urinary tract clear.
- Practice good hygiene: Wipe front to back to help avoid spreading bacteria, and choose gentle cleansers that won’t irritate your sensitive areas.
- Go when you need to: Don’t hold it in! Giving your bladder regular breaks helps keep things flowing.
- Pee after sex: This helps flush out anything that might have been introduced during intimacy.
These small adjustments to your lifestyle can make a real difference, especially if you’re someone who deals with recurring UTIs. And if you want to take it a step further, consider keeping a journal to track any changes you notice in bathroom habits or sensations—sometimes seeing patterns can help guide the next steps.
Dietary Tips
What you eat can play a role in how your bladder feels. The good news is that you can take charge by making a few simple tweaks:
- Eat nutrient-rich foods: Fresh fruits, vegetables, and whole grains provide essential vitamins and antioxidants that support your body’s natural defenses.
- Cranberries (in moderation): While they’re not a cure-all, some people find that unsweetened cranberry juice or supplements can help support bladder health. Just be sure to watch for added sugars!
- Limit sugary snacks and drinks: Foods high in sugar can create a friendly environment for bacteria, so cutting back on sweet treats can be helpful for your urinary health.
- Consider probiotics: Found in foods like yogurt or supplements, probiotics can help support the balance of good bacteria in your gut, which also plays a part in urinary function.
Eating well isn’t just about fueling your body—it’s about feeling good and staying strong. And when it comes to your bladder, healthy food choices make a big impact.
Hydration is Key
Hydration is one of the easiest ways to support your urinary health, especially during menopause, when fluid balance can be a little more tricky. Water helps flush out potential invaders and keeps things moving.
Here are some simple hydration tips:
- Sip regularly throughout the day: Instead of drinking large amounts all at once, try sipping a little water every hour. It’s a lot easier on your body.
- Add some flavor: If plain water gets boring, try herbal teas or water with a splash of fruit juice to keep things interesting.
- Create a routine: If you struggle with hydration, set a reminder to drink a glass of water each hour. This can help make it a habit.
Hydration is especially important if you’re dealing with menopause-related dryness. Drinking enough water helps keep everything balanced and supports your kidneys and bladder. Staying hydrated means your body can do its job—and so can you.
Can Menopause Cause Recurring UTIs?
Frequent UTIs can happen in menopausal women due to a decline in estrogen combined with menopause-related changes such as weakened bladder muscles, urinary retention, and pelvic organ prolapse. It can make it harder to empty the bladder, allowing bacteria to multiply and cause infections.
These combined factors increase the risk of recurrent UTIs in postmenopausal women. Seek medical help if you experience frequent UTIs, blood in the urine, fever, back pain, or symptoms that do not improve with treatment.
Treating UTIs During Menopause
No matter how mindful you are about your urinary health, UTIs can still happen. When they do, acting quickly can help you recover faster and feel more comfortable. Menopause can bring some unique challenges, like hormonal changes that can slow down the body’s natural healing process. That’s why it’s important to work with a healthcare provider who understands menopause and your body’s specific needs.
Getting an Antibiotic Prescription
When an infection strikes, prescription antibiotics for UTIs are the go-to treatment, especially if tests show bacterial involvement. These medications target the bacteria causing the infection, helping your body heal. It's important to follow your provider’s instructions and finish the full course of antibiotics—even if you’re starting to feel better.
For pain relief, over-the-counter medications might be an option, but it’s best to check with your clinician for guidance on what will work best for you.
Wisp treatment options are available only after consultation with a licensed medical professional. You should consult with your healthcare provider before starting a new supplement or treatment regimen. Individual results may vary.
The Role of Additional Treatment
Antibiotics are a key part of UTI treatment. Your provider might prescribe a short course, typically 3 to 5 days, or a longer one if the infection is more severe.
However, in menopausal and postmenopausal women, some clinicians may also discuss adding topical estrogen or other treatments to support thinning tissues, which can be a factor in frequent UTIs.
Certain strains of probiotics can be a helpful addition to your urinary health management toolkit, as they could help balance good and bad bacteria in your body—especially if you’re taking antibiotics.
Since everyone’s body responds differently, your provider will guide you in finding the right approach.
Exploring Natural Aids
If you’re looking for a natural approach to help your body along, there are some options to consider. Probiotics, vaginal moisturizers, and supplements like D-mannose can all be helpful for supporting urinary health.
While these options won’t replace antibiotics for moderate or severe infections, they can be great as part of a well-rounded plan to support your vaginal microbiome and help with handling your day-to-day health.
Simple at-home remedies, like warm compresses or heating pads, can help soothe discomfort by relaxing the muscles around your bladder and easing the twinges that come with a UTI. Many people find that combining both medical treatments and natural vaginal support aids can offer the best balance for healing and staying well.
The Benefits of Estrogen Therapy
Estrogen therapy could offer some relief for those experiencing frequent UTIs, especially after menopause, when hormonal changes can make tissues around the urethra and bladder more delicate.
While it may not be the right choice for everyone, it’s an option worth exploring for individuals who struggle with recurrent urinary tract infections.
How Estrogen Therapy Works
During menopause, the protective layers of tissue around the urethra and bladder can thin, making it easier for bacteria to take hold.
Estrogen therapy helps rebuild these layers, offering a stronger barrier to bacterial infections. This can lead to fewer opportunities for bacteria to cause UTIs and may also help with dryness or irritation in intimate areas. It’s a fresh coat of paint, restoring some of the natural strength of tissues that have weakened over time.
Different Forms of Estrogen Therapy
There are a few ways to apply estrogen, and the best option depends on what works for your body.
Vaginal creams allow you to target the hormone directly to the area where it's needed, while vaginal rings release the hormone gradually.
Vaginal tablets offer another controlled dose option.
Each method has its own benefits, so it’s important to discuss your preferences and medical history with your healthcare provider to find what works best for you.
Potential Risks and Considerations
Estrogen therapy isn’t for everyone, and it’s important to consider your health history, especially if you have a personal or family history of certain conditions like cancer or clotting disorders.
Finding the right dosage is key, so regular follow-ups with your provider are important. If estrogen therapy doesn’t align with your needs, there are alternatives, like moisturizers or probiotics, that could offer support in managing UTIs.
Always have open conversations with your healthcare provider to explore the best approach for you.
When to Seek Medical Help
UTIs can sometimes feel like a mild inconvenience, but they can also escalate quickly, especially during menopause, when your body’s usual signals might be harder to read. It’s important to know when to reach out for medical care to avoid complications. The sooner you address a UTI, the easier it is to avoid serious issues like kidney or bloodstream infections.
Recognizing Serious Symptoms
Certain symptoms can indicate that a UTI is becoming more serious.
If you’re experiencing strong chills, a high fever, or pain in your sides or back, these could be signs that the infection is spreading.
Blood in your urine that doesn't improve is another serious red flag. If you feel lightheaded, can’t pass much urine, or are vomiting, don’t wait—contact a healthcare provider right away. Prompt action can help you avoid bigger issues.
Consulting with a Healthcare Provider
Your provider may want to run some tests to determine which bacteria are causing the infection or check for any structural abnormalities, such as kidney stones or blockages. This is especially important if UTIs are happening frequently.
It’s also a good time to discuss how menopause may be affecting your bladder health, as hormonal changes can contribute to recurrent UTIs.
Managing UTIs Curing Menopause
Taking care of your bladder health during menopause is part of embracing your body’s natural changes. As hormone levels shift, you may notice some differences in how your body responds to bacteria. But that doesn’t mean UTIs have to be a constant companion.
Being proactive about spotting early symptoms and following your healthcare provider's advice can make a big difference in keeping UTIs at bay, allowing you to focus on the positives of this new life stage. Menopause doesn’t have to be defined by constant infections—empowerment starts with knowledge.
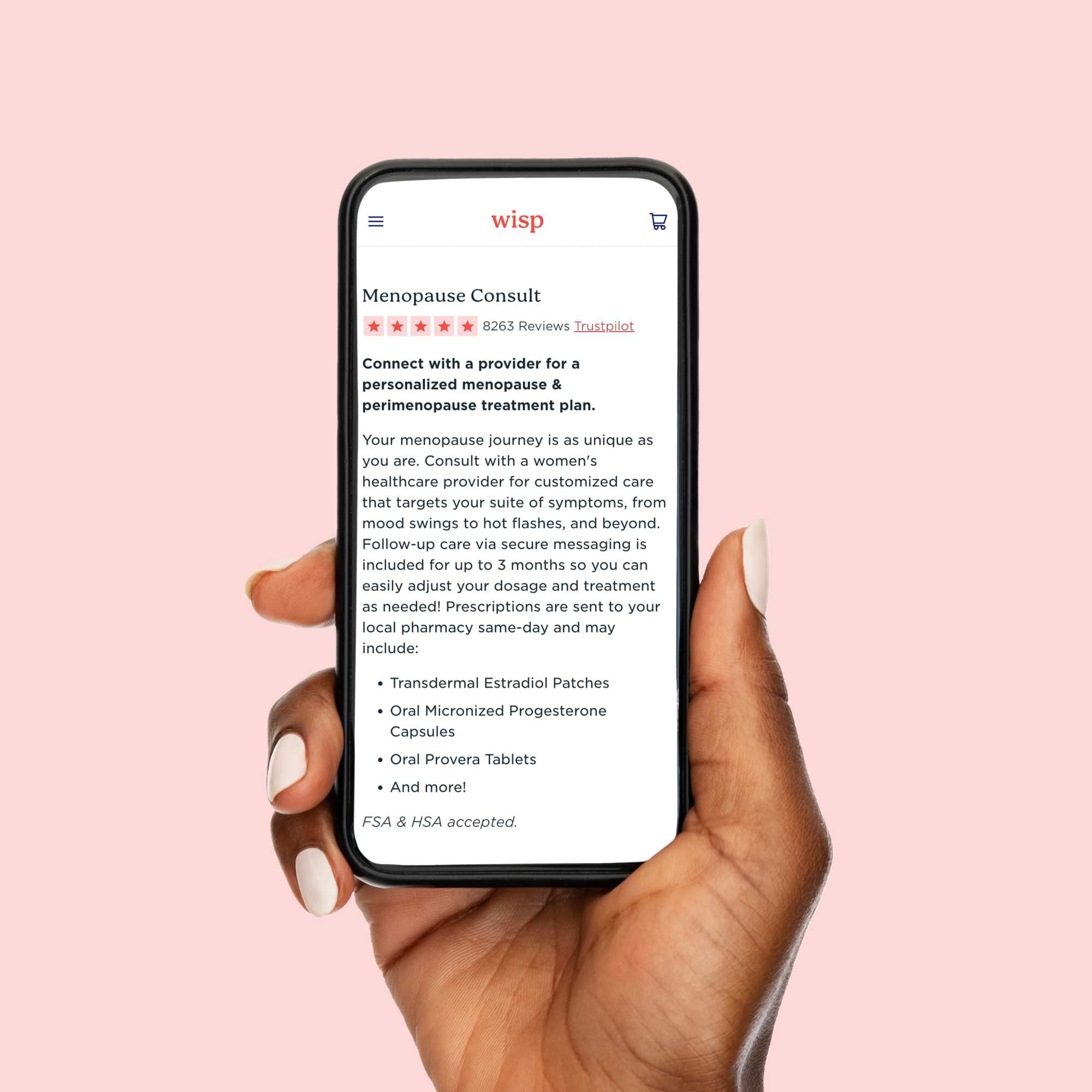
Need support? At Wisp, we’re here to help you take charge of your health every step of the way. Whether you’re managing a UTI, navigating menopause, or just have questions about your body, we’ve got you covered. Expert guidance, discreet care, and simple solutions. We’re here for you—whenever you’re ready.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.