
Managing Perimenopause Sleep Issues
Published on August 26, 2025
Written by Kathleen Morrison
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
If you’ve been lying awake at 2 a.m., sweaty, restless, and wondering what the heck is going on with my body?—it could just be your hormones. Perimenopause (aka the hormonal rollercoaster that leads up to menopause) can totally mess with your sleep. Think night sweats, hot flashes, mood swings, and sudden anxiety. Basically, a full-body group chat you didn’t ask to join.
Here’s the deal: as estrogen and progesterone levels shift, your sleep cycles can get thrown out of whack. These hormones don’t just affect your period; they’re also major players in how easily you drift off and stay asleep.
But just because your hormones are doing the most doesn’t mean you have to suffer through sleepless nights. Small shifts can make a big difference, like sticking to a regular wind-down routine, cooling down your sleep space (shout out to fans and light bedding), and keeping your room calm and cozy.
Why is perimenopause messing with my sleep?
Let’s start with the why. During perimenopause, your hormone levels (particularly estrogen and progesterone) fluctuate significantly, and those changes can seriously disrupt your body’s natural sleep-wake cycle.
Estrogen may not directly affect your sleep, but it plays a key role in regulating your body temperature and influencing serotonin levels, which help control your sleep patterns. When estrogen dips, you might experience night sweats, increased body temperature, and mood changes, all of which make it harder to fall asleep or stay asleep.
Progesterone, sometimes called the body’s natural sleep aid, has a calming effect. When levels drop during perimenopause, you might notice more restlessness or even insomnia.
To make things more frustrating, these hormonal shifts don’t follow a neat schedule, they’re unpredictable. That means one night you might sleep fine, and the next you’re tossing and turning until sunrise. Add in stress, anxiety, or physical symptoms like hot flashes, and you’ve got a perfect storm for sleep disruption.
So if you’re waking up exhausted or lying awake at 3 a.m. wondering what’s going on, know that it’s not just in your head—your hormones really are in flux, and sleep struggles are a very real part of the perimenopausal experience.
Common sleep symptoms during perimenopause (And what they actually feel like)
Struggling to get a good night’s sleep lately? If you’re in your 40s or 50s, shifting hormones might be to blame. Perimenopause—the transitional phase before menopause—can throw your sleep patterns out of whack in ways that are frustrating, confusing, and downright exhausting. Let’s break down the most common symptoms and what they really feel like (because they’re not always what you’d expect).
Night sweats and hot flashes
Sudden waves of heat in the middle of the night? Yep, those are hot flashes, and they’re one of the most disruptive menopausal symptoms. They can leave you sweaty, chilly, and wide awake.
- Hot flashes vary in intensity. Some feel like a warm flush, others like your body’s on fire
- They can mess with your sleep quality by waking you up and further messing with the little bit of sleep you do manage to get
- Keep your room cool, wear light layers, and try moisture-wicking sheets
The “wired but tired” feeling
You know that feeling where you’re exhausted, but your brain is doing cartwheels? That’s common in perimenopause, too. Hormonal shifts can affect neurotransmitters like serotonin, making it harder to wind down and leading to poor sleep.
- Falling asleep feels impossible
- Staying asleep is just as tricky (hello, 3 AM wakeups)
- A soothing bedtime routine (like light stretching or reading) can really help
Restless legs and feeling fidgety
Some folks also deal with restless legs syndrome or general physical unease. It’s like your body’s too antsy to settle, even when your brain wants to sleep. This is super common in middle-aged women and often overlooked.
What’s actually happening in your body?
Let’s get into the science-y part of perimenopause sleep problems (without the jargon). Sleep disruption during perimenopause isn’t just about night sweats—it’s about deeper hormonal shifts that affect your sleep architecture.
Estrogen, progesterone, and sleep quality
When estrogen dips, your body’s ability to regulate temperature, mood, and stress takes a hit. Progesterone (which has a calming effect) also drops, and that combo can seriously mess with your ability to fall and stay asleep.
FSH and cortisol
- FSH (follicle-stimulating hormone) ramps up in perimenopause, and high levels are linked to sleep issues
- Cortisol (your stress hormone) might spike at night instead of calming down like it’s supposed to, leaving you restless
- Thyroid function may shift, too, and even minor imbalances can lead to more trouble sleeping
How hormone therapy could help you sleep better
Menopausal hormone therapy (MHT) is one of the go-to options for tackling those pesky perimenopausal symptoms, especially when it comes to getting better sleep. Estrogen treatments can calm down hot flashes for loads of people, making nights way more comfortable.
There are different ways to take hormones, and each comes with its perks. Transdermal patches, for example, deliver a steady dose throughout the day, helping your body feel more balanced. Bioidentical progesterone? It’s known to have gentle calming effects that might help you drift off more easily.
Experts suggest starting hormone therapy around the time perimenopause kicks in to get the best results.
Lifestyle shifts that might help you sleep
Perimenopause can mess with your sleep, but you’re not stuck tossing and turning forever. A few intentional changes to your routine can help make a difference, especially when you stick with them. Think of these like tools in your personal sleep toolkit: not one-size-fits-all, but worth trying to see what feels right for you.
Movement and nutrition
The way you fuel and move your body plays a bigger role in your sleep than you might think.
- Magnesium is your sleepy-time BFF: you’ll find it in leafy greens, almonds, cashews, avocado, and even dark chocolate.
- Watch the caffeine clock: your tolerance might shift in perimenopause, so it’s a good idea to wrap up your last cup before 2 PM.
- Movement matters: aim for 30 minutes of something that gets your body going most days. Morning movement is even better (hello, natural light and circadian rhythm support).
You don’t need to suddenly become a wellness influencer. Just tune in to what helps your body feel balanced and grounded.
Bedtime rituals
A predictable wind-down routine isn’t just cozy, it’s one of the best signals you can send your body that sleep is on the way.
- Start dimming the lights around 60–90 minutes before bed to cue melatonin.
- Swap the scroll for something soothing like stretching, journaling, or your favorite book.
- Take a warm shower an hour before bed—your body cools down afterward, which can help you drift off easier.
- If night sweats strike, keep water and a small towel by your bed so you can cool off quickly and get back to sleep.
Consistency is key here. The more you show up for your sleep routine, the more your body will start to adjust.
Manage stress
Stress loves to mess with your sleep, especially during perimenopause when hormones are already doing their thing. Carving out a few minutes each day for mindfulness, meditation, or simple deep-breathing exercises can help calm your mind and body.
Try these:
- A quick guided meditation before bed
- Deep belly breathing to ease tension
- Journaling your thoughts to clear your head
Building these into your daily routine can help ease that “wired but tired” feeling and make falling asleep a whole lot easier.
When to seek professional help
Sometimes, sleep struggles just won’t quit, even after trying lifestyle tweaks. If your sleep troubles stick around for more than three months, it might be time to chat with a pro.
Keep an eye out for signs like feeling wiped out all day and it’s messing with your work or life, really loud snoring that could hint at obstructive sleep apnea, or restless movements that won’t let you settle down at night. It’s super helpful to jot down your sleep patterns and how often those pesky hot flashes hit before your appointment. This gives your provider the full picture.
Treating perimenopause sleep issues usually takes a well-rounded plan. Your provider might suggest hormone therapy, talk therapy like cognitive behavioral therapy for insomnia (CBT-I), or a mix of approaches. For simplicity, online consultations can get you connected with experts who get it and can guide you through a plan that fits you perfectly.
Sweet dreams and sleep health
Tackling perimenopause sleep issues can take patience—and sometimes a little extra help. Remember, your journey is totally your own, and what works for someone else might not be your perfect fit.
Building good sleep habits now pays off long after perimenopause has passed. Believe it or not, restful nights are within reach with the right mix of tools, tweaks, and support. When you take charge of your sleep, you’re also boosting your overall well-being during this big life transition.
Ready to take the next step? Wisp is here with expert care tailored just for you—offering personalized consultations and convenient options that make managing perimenopause easier and more approachable than ever. Because you deserve nights full of rest and days full of energy.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.
Frequently Asked Questions (FAQ):
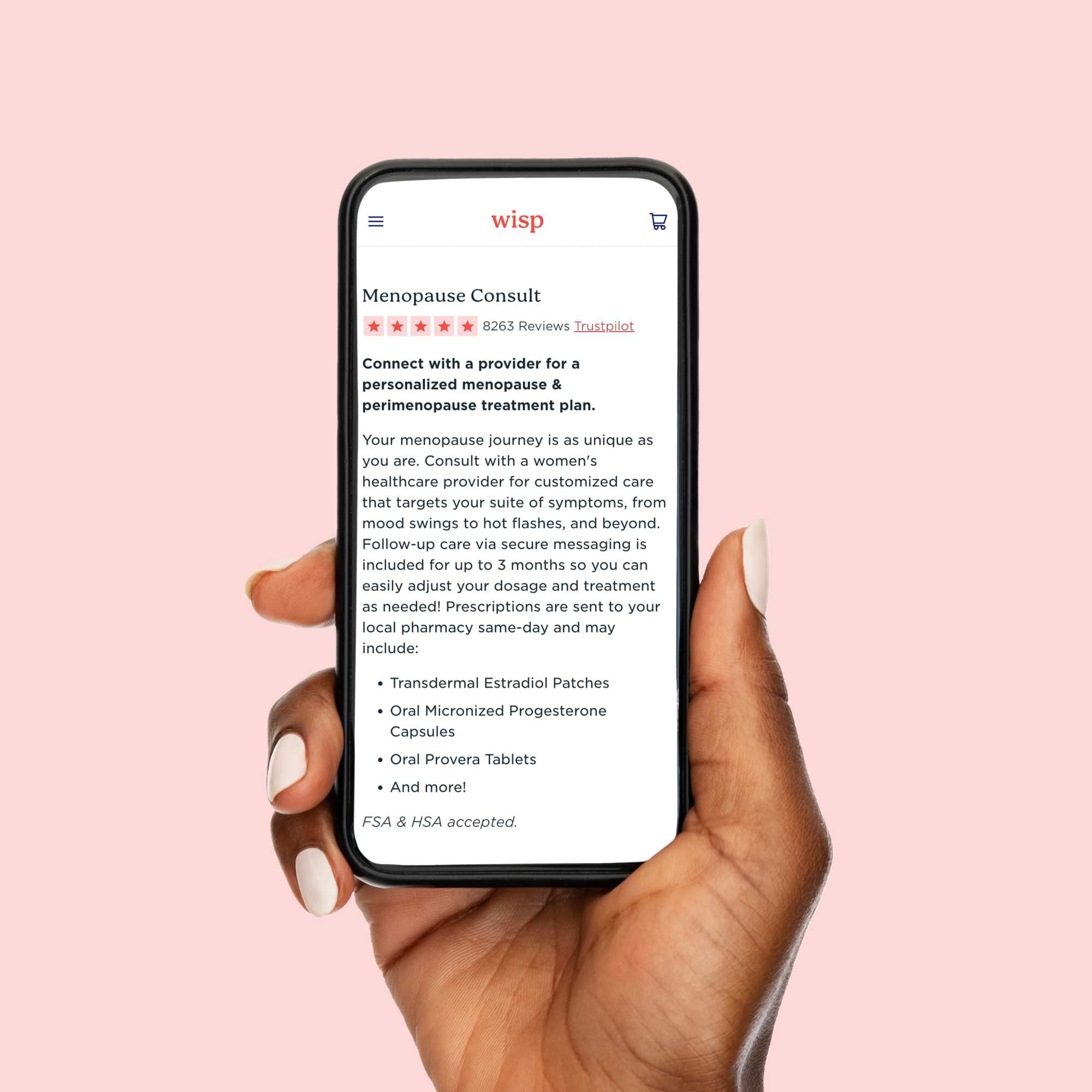
Menopause Consult
$99
Customized care for menopause & perimenopause symptoms including estrogen & progesterone hormone replacement.


