
Telehealth: A Timely
(and Discreet) Solution
To The American Health
Insurance Gap
By Viggy Hampton
January 16, 2024
Every American will need medical care at some point in their lives. For many, accessing needed care is simple—but for over 25 million non-elderly Americans without health insurance, even a simple in-person licensed medical provider visit can be an insurmountable cost.
When cost is a barrier to access, over 20% of uninsured adults forgo necessary clinical care because of cost. Even for those who can easily access care, the “stigma” or fear of awkward conversations with unfamiliar doctors prevents some from seeking treatment for common issues ranging from routine reproductive care, inflammation, and STI screening.
Because of high costs and frustrating stigma, ignoring symptoms is a way of life for many Americans. Instead of treating infections early, millions of Americans suffer in silence, resulting in expensive emergency room visits and advanced disease states.
In the face of these issues, telehealth has stepped in as a more flexible, affordable, and discreet option for those with insurance and those without. Telehealth can’t replace annual in-person medical exams for running biometrics and spotting the early warning signs of disease. However, telehealth makes it simpler to access medication and treatment between annual exams—especially for those too embarrassed to discuss their sexual health in person—and provides a life raft for the many Americans with no viable health coverage to speak of.
Benefits of Telehealth Over Traditional Healthcare
Before telehealth was an option, accessing care for common issues like urinary tract infections (UTIs) or genital herpes outbreaks was often expensive, time-consuming, and frustrating. Taking time off work, sitting in waiting rooms, taking costly tests—all for a diagnosis you already know you have.
For many, telehealth offers a more convenient and affordable path to receiving a diagnosis and necessary treatment than traditional healthcare. With the recent explosion of telehealth options, you can now:
- Speak with a medical provider from the comfort of your home
- Receive a diagnosis online or referral to an in-person clinic when needed
- Have your much-needed prescription sent to your local pharmacy or delivered directly to your door
- Complete all of the above, regardless of your insurance
Who Can Benefit from Telehealth?
If you are one of the millions of Americans who must choose between an in-person medical provider visit and taking off work or dipping into savings and credit just to get treatment, you’re not alone. With no known cure, over 572,000 people are diagnosed with genital herpes each year, and uncomplicated UTIs are among the most common bacterial infections plaguing Americans today.
To make matters worse, many women who are diagnosed with a UTI have a recurrence within six months. It doesn’t feel right to have to go through the inconvenience and expense of an urgent care visit just to be told what you already know. Medication for urinary tract health and other conditions shouldn’t be so difficult to access. If you have experienced any of these frustrating situations, telehealth is here to help.
Healthcare Can Be a Serious Financial Burden
Healthcare in our current system doesn’t come cheap, even for people who have insurance. For those who don’t, finding affordable healthcare when you need it can be next to impossible.
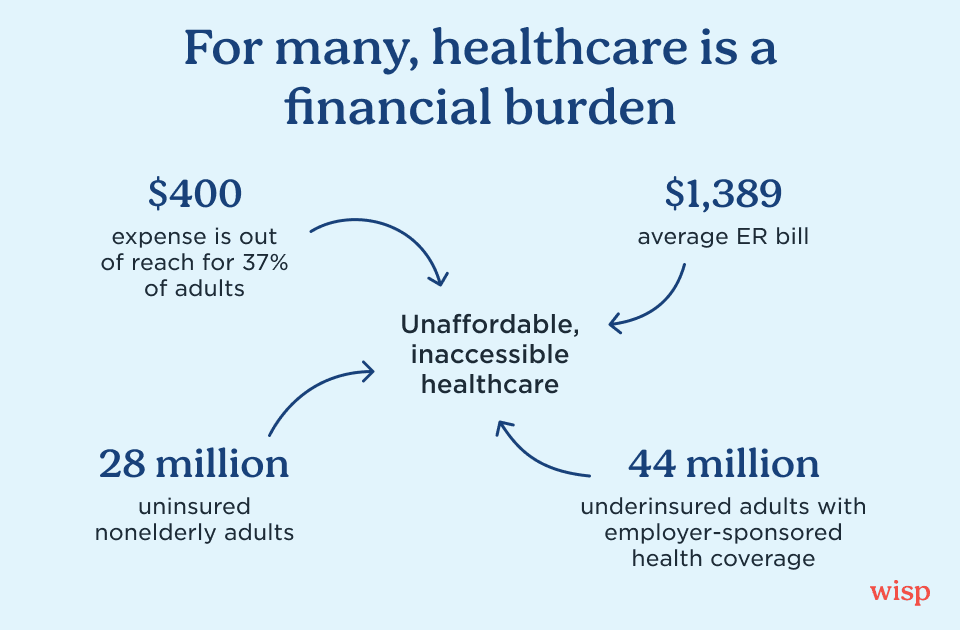
In 2023, the percentage of uninsured adults hit historic lows at 9.5%. This is a huge step in the right direction...or so it seems. Even though there are fewer uninsured Americans, 23% of adults have insurance that doesn’t fully pay for the health costs they need covered–leaving them underinsured.
What does it mean to be underinsured? Underinsurance means that you have some health coverage, but for some reason—such as high deductibles or high out-of-pocket costs—you still have difficulty paying your medical bills. Unfortunately, receiving health insurance through your employer doesn’t save you from being underinsured. In fact, 66% of underinsured adults have coverage through an employer plan, and 14% have coverage through the individual market.
In 2023, a survey by the Federal Reserve found that 37% of adults would be unable to pay a $400 expense using cash or its equivalent. That’s especially problematic when the average cost of an emergency room (ER) visit in 2019 was $2,453. Besides that, 23% of adults in 2023 had major, unexpected medical expenses that averaged between $1,000 and $1,999.
What does all of this mean? For the sizable population of uninsured or underinsured folks, accessing and paying for needed treatment becomes a choice between treatment and paying the rent. While it can’t solve everything, this is where affordable telehealth options can certainly help.
How Telehealth Can Fight Against Stigma
Beyond the financial burden of accessing healthcare, many conditions related to reproductive health are stigmatized. This stigma may lead some to delay seeking treatment. In the case of STIs, like Genital Herpes or Chlamydia, carriers may not know they have the infection and therefore make no lifestyle change to prevent further transmission to unsuspecting sexual partners.
When left untreated, other easily treatable conditions can accelerate rapidly and may lead to hospitalization (like a run-of-the-mill UTI becoming a kidney infection) and costly Urgent Care bills (remember that ridiculously high average ER cost of $2,453?).
When shame, stigma, and stress team up with inaccessibility and high costs around some of the most common reproductive health conditions, the result is a culture of untreated illness that can only lead to more suffering.
Luckily, there’s a solution: enter telemedicine. Legions of licensed medical providers have moved online, where the overhead costs of providing care are lower. There, telehealth companies connect patients with the resources they need, at an inclusive price point, which opens the door for millions of underinsured Americans to get treatment.
What Is Telehealth?
In short, telehealth describes the use of communication, video, and other technologies to connect patients to healthcare, sometimes over long distances. Video-chatting with a physician, forwarding data from your Fitbit to your care team, having your primary care provider consult with a specialist in another state, and receiving prescriptions online are all forms of telehealth.
Now that many patients have their first telehealth experiences under their belts, telehealth demand will likely grow. Just think—if you could talk to your therapist, your primary care physician, and your specialist all from the comfort of your own home, would you really miss going back to a crowded waiting room and sitting, reading old magazines, until your care provider was finally ready to see you?
Specialists In Reproductive Health
Telehealth is quickly making inroads to address the specific issues of access and discreet care for specific conditions that prove most troublesome for Americans. Providers like Wisp, an online community for female and male reproductive health, specialize in making care more accessible and affordable via a stigma-free, online platform.
Accessing Wisp care is simple, and a US-licensed medical provider will review your symptoms and prescribe care if safe and appropriate. Their medical team treats patients in all 50 states and provides prescription medication, over-the-counter remedies, and STI consultation—whenever and wherever you need it.
Leveraging Telehealth to Bring Affordable Care to You
Wisp provides all the benefits of telehealth—convenience, accessibility, speed—along with:
- Eco-friendly discreet packaging
- An online resource center to help answer all of your burning questions
- Affordability
- A free Wisp x GoodRx card for extra savings on prescriptions
- No insurance required
How does telehealth work? Well, if you needed treatment today for herpes, for example, here’s how that process works with Wisp. Head to Wisp’s website and choose your medications using a quick online form. Within 24 hours, a Wisp licensed medical provider reviews your order and prescribes personalized treatment. You can choose free medication delivery in Wisp’s discreet eco-friendly packaging or have it sent to your pharmacy within 3 hours of completing your medical intake form and phone call or video chat when necessary. Questions? Reach out to chat with Wisp’s pharmacy or medical team.
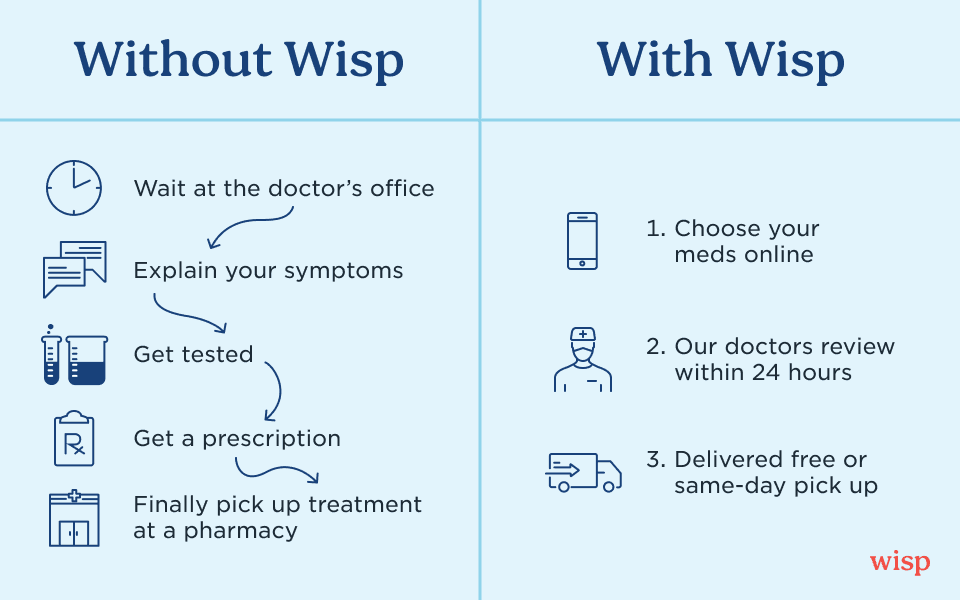
No more sitting in a crowded waiting room for hours, explaining uncomfortable symptoms to yet another medical provider, paying for a diagnostic test you don’t need, deferring care because it’s too expensive, or hiding your medications from prying eyes. Wisp combines convenience, discretion, quality clinical care, and budget-friendly access to necessary prescription treatments and preventive products.
Wisp Is Growing Every Day!
As Wisp expands in response to the United States’ healthcare needs, our ability to keep you healthy will only grow. We’re happy to provide birth control, skin care, STI treatments, menopause support, weight care, and more–all available quickly and conveniently online.
With Wisp, you also have access to online consultation, a service we offer for patients unable to get to an in-person medical provider for basic care needs. We can also order your lab test to get screened for sexually transmitted infections (STIs), which is especially helpful in certain states that underfund Planned Parenthood and free clinics. As a telehealth provider, Wisp is in your corner–and we’re here to stay.
Learn more about Wisp here, and begin your journey to better health by taking our Symptoms Quiz.


