What Is Menopause and
What Can You Expect?
Published on September 26, 2024
Updated on October 3, 2025
Written by Kathleen Morrison
Medically Reviewed by Andrea Sleeth WHNP-BC, MSCP
Key takeaways:
- Menopause is a natural milestone: your periods stop, hormones shift, and your body enters a new chapter. Timing and symptoms vary for everyone.
- Common changes include hot flashes, night sweats, mood swings, sleep struggles, vaginal dryness, and shifts in metabolism, bone, heart, and urinary health.
- Perimenopause can start years before your last period, with irregular cycles and fluctuating hormones. Paying attention to your patterns helps you navigate the transition.
- Lifestyle tweaks like moving your body, eating mindfully, and managing stress can make a big difference in how you feel day to day.
- Hormone therapy and nonhormonal treatments are available for moderate to severe symptoms—but what’s right depends on your health, preferences, and guidance from a healthcare provider.
- Keep an eye on unusual or severe changes (like heavy bleeding, disrupted sleep, or mood swings affecting your life) and don’t hesitate to reach out for professional support. Getting help is proactive, not a weakness.
Menopause is a big milestone in a person’s life—it’s when your periods stop for good, usually somewhere between your mid-40s and mid-50s. And yes, it comes with a whole mix of changes. Some you might notice physically, some emotionally, and some that sneak up on you.
Menopause happens because your hormone levels, like estrogen and progesterone, shift. That can bring on things like hot flashes, mood swings, and sleep disturbances, but remember, everyone’s experience is different. There’s no “one-size-fits-all” way to go through it.
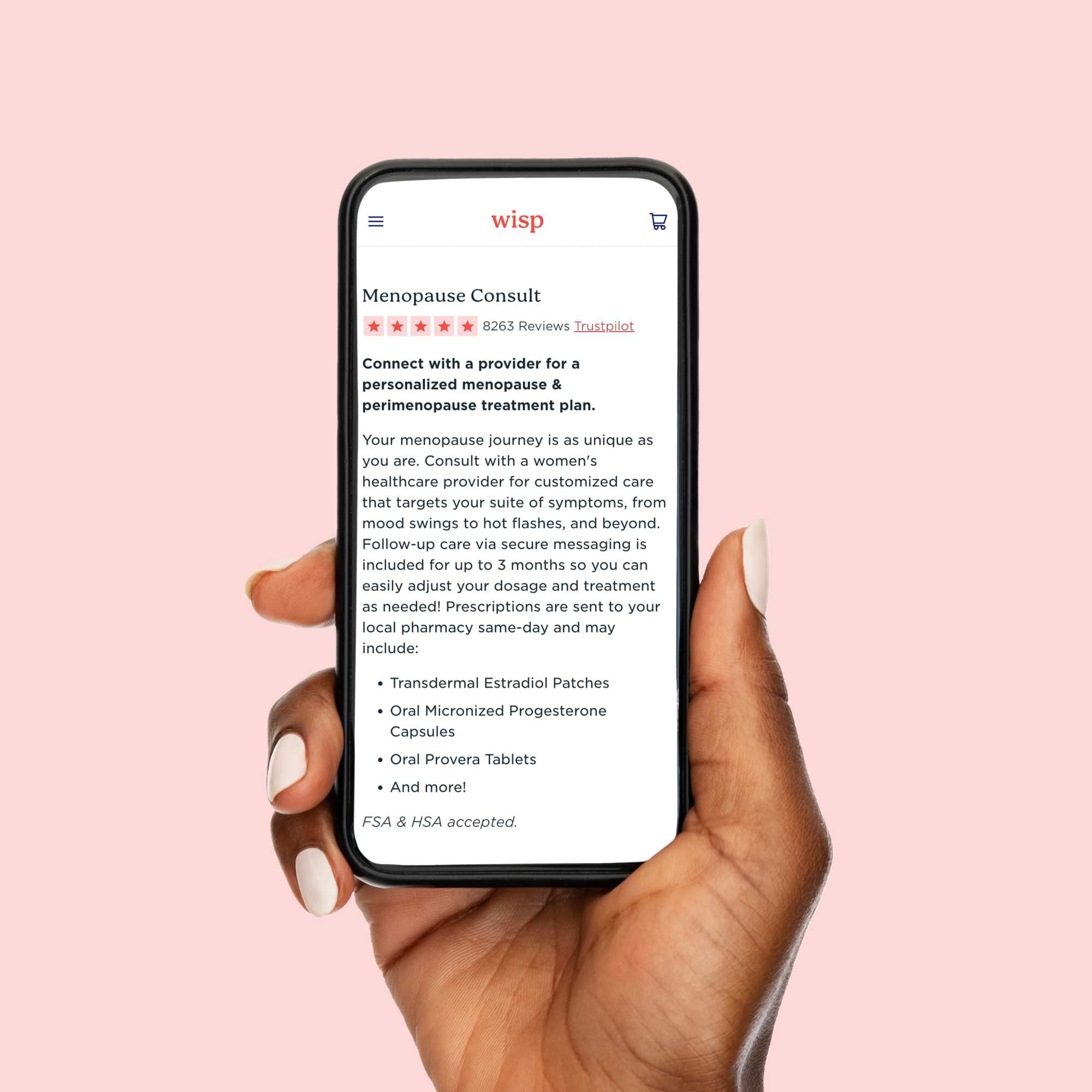
What can help? Trying new routines that make you feel good can really change the game. Think nourishing your body with foods that make you feel energized, moving in ways that feel fun, and carving out time to unwind. Consulting with a Wisp provider can help address your curiosity and provide customized care, allowing you to feel more confident, comfortable, and in control of this next chapter.
Why does menopause happen?
Menopause happens when your ovaries slow down hormone production, specifically estrogen and progesterone (the hormones that drive your menstrual cycle). It’s a natural transition from your reproductive years to the post-reproductive phase of life.
Here’s the scoop:
- Ovaries in action: During your reproductive years, your ovaries release eggs each month and produce hormones that get your body ready for a possible pregnancy.
- Hormone changes over time: As you get older, your egg supply drops, and hormone production gradually declines. This doesn’t happen overnight... It’s a slow shift that can span years or even decades!
- Timing varies: Genetics plays the biggest role in when menopause arrives, but lifestyle and health also matter. Smoking can speed things up, certain medical conditions can bring menopause earlier, and some people experience sudden menopause due to surgery or treatments like cancer treatments that affect ovarian function.
Understanding why these changes happen can make the journey feel a little less mysterious and a lot more manageable. Your body's just moving into a new chapter.
When does menopause start?
Menopause doesn’t have a set start date; it’s different for everyone. Most people notice it between their mid-40s and mid-50s, with the average age in the U.S. around 52. But your genetics, lifestyle, and overall health all play a part, so your timing might be a little earlier or later, and that’s totally normal.
Before menopause officially kicks in, there’s a phase called perimenopause, which can start in your late 30s or 40s. Hormones are on a bit of a wild ride during this time, so it's really common to notice irregular periods. Some months you might skip one entirely, and other months they might be heavier or just different than usual. This phase can last anywhere from a few months to over a decade, so it’s all about noticing patterns and listening to your body.
You officially reach menopause after you've gone a full 12 months without a period. (And yes, you should totally throw a party). From that point on, you’re considered postmenopausal.
Some people reach these milestones earlier than others. "Early menopause" is when this happens between 40 and 45 (this happens to about 5% of women), while "premature menopause" occurs before 40 (around 1% of women). These earlier transitions can happen for lots of reasons, like genetics, autoimmune conditions, or medical treatments like chemotherapy. Even lifestyle factors, like smoking, can make menopause arrive a bit sooner.
Common symptoms of menopause
Menopause symptoms affect most women, but how they show up is very personal. Hormones, especially estrogen, shift during this phase, which can impact nearly every part of your body. Some people sail through with barely a hiccup, while others notice bigger (more unpleasant) changes.
Hot flashes and night sweats
Hot flashes and night sweats are a classic part of the menopausal transition. Here’s what to know:
- Hot flashes: Sudden waves of heat starting in the chest or face, lasting seconds to minutes. You might feel flushed, sweaty, or anxious, followed by chills.
- Night sweats: Hot flashes during sleep, which can soak pajamas and sheets and leave you exhausted the next day.
- Frequency & triggers: Some people get a few mild flashes weekly, others experience several intense ones every day. Triggers often include spicy foods, caffeine, alcohol, stress, or warm rooms. Keeping a quick symptom diary can help you spot personal patterns.
Mood shifts and sleeping trouble
Hormone changes can affect your emotions and sleep. Common experiences include:
- Mood swings: Feeling more irritable, anxious, or emotional than usual. Little annoyances can feel overwhelming, and swings can happen quickly.
- Sleep disruption: Night sweats and hormonal shifts can make falling or staying asleep tricky, leading to fatigue, brain fog, and increased emotional sensitivity.
- Tips: Small adjustments to bedtime routines and sleep environments can help, and talking openly about these changes can also help normalize the experience. You're not alone in this!
Vaginal dryness and discomfort
Intimate changes are really common (known as genitourinary symptoms), and they can affect your daily comfort and sexual activity, too. Watch out for:
- Dryness & thinning tissue: Vaginal tissues become thinner and less elastic, reducing natural lubrication, making sexual intercourse a little uncomfortable.
- Other changes: pH shifts, increased irritation, and more delicate tissues can cause discomfort or occasional bleeding.
- Solutions: An estradiol vaginal cream or non-hormonal vaginal moisturizer can help provide some targeted relief and help you feel a little more comfortable and confident again.
Wisp treatment options are available only after consultation with a licensed medical professional. You should consult with your healthcare provider before starting a new supplement or treatment regimen. Individual results may vary.
How does menopause affect your health?
Menopause isn’t just about your periods stopping. Hormones like estrogen influence nearly every system in your body. When estrogen dips, it can affect your metabolism, bones, heart, and urinary health.
Metabolism
During menopause, your metabolism can slow down, which sometimes makes weight management a little trickier. Fat often redistributes to your midsection, and this isn’t just about looks—it can increase risks for conditions like diabetes and heart disease.
It’s normal to feel frustrated when your usual diet and exercise routines don’t work the same way, but small lifestyle tweaks and awareness can help make a difference.
Bone health
Estrogen helps keep your bones strong by slowing natural bone breakdown. When estrogen drops, bone loss speeds up—women can lose up to 20% of bone density in the five to seven years after menopause.
- Bones can get fragile, increasing fracture risk, especially in the hip, spine, and wrist. Hip fractures are serious and can affect independence and overall health.
- Bone loss is often silent, which means you might not feel it until you end up with a fracture. That’s why bone density tests during and after menopause are super important. Early detection can help give you a clear picture and open up options to maintain your bone health from the get-go.
Heart health
Cardiovascular disease becomes a major health risk after menopause. Estrogen before menopause helps keep cholesterol levels balanced, blood vessels flexible, and blood pressure in check. After menopause:
- LDL (bad) cholesterol can rise, HDL (good) cholesterol may drop.
- Blood vessels stiffen, and blood pressure can creep up, even in women with no history of hypertension.
- Women with early menopause face even higher risks, and frequent or severe hot flashes might signal blood vessel changes.
Being aware of these shifts gives you a heads-up to monitor your heart health and stay proactive.
Urinary health
Estrogen affects the tissues in your urinary system, so hormonal changes during menopause can cause:
- Urinary incontinence: Up to 50% of postmenopausal women experience leaking when coughing, sneezing, or exercising (stress incontinence) or sudden urgent urges (urge incontinence).
- Recurrent urinary tract infections: Shifts in vaginal pH can allow harmful bacteria to flourish. Post-menopause UTIs can sometimes look different than before, presenting as fatigue or confusion rather than classic burning or urgency.
Knowing these changes are common helps you feel prepared, and discussing symptoms openly can lead to effective ways to manage them with confidence.
How to manage menopause symptoms
Managing menopause isn’t about just getting through it, it’s about finding what helps you feel your best. There’s no one-size-fits-all solution, so discovering your ideal mix of approaches takes a little trial and error.
The trick is addressing both immediate symptoms and long-term health. Hot flashes might need quick attention, but thinking about preventing osteoporosis and looking after your overall wellness matters too. A plan that fits your symptoms, health history, and lifestyle will give you the most comfort and confidence. An online menopause consult followed by a tailored treatment plan can help women figure out what works for them.
Lifestyle and diet changes
Small lifestyle tweaks can help make a difference to how you feel during menopause:
- Move your body: Regular exercise can help with hot flashes, mood, sleep, and bone strength: a nice all-rounder. Try to aim for at least 150 minutes a week, mixing cardio and strength training.
- Eat mindfully: Diet affects how you feel inside and out. Some people may notice fewer hot flashes when they limit caffeine, alcohol, and spicy foods. Including foods like soy, flaxseeds, legumes, and following a Mediterranean-style diet can help support your overall health.
- Stress relief: Stress can make all your symptoms feel just that little bit worse (or even a lot worse). Yoga, meditation, deep breathing, or any activity that lets you unwind can help improve both how you feel physically and emotionally. Many women find great new coping strategies during menopause that stick with them for life.
Hormone therapy options
Hormone therapy can be really effective for moderate to severe symptoms, like hot flashes and vaginal dryness. Most modern approaches use the lowest effective dose for the shortest time needed, to keep a good balance between benefits and side effects.
- Forms: Pills, patches, gels, and sprays are available. Patches bypass the liver, gels let you adjust your dose, and your choice depends on preferences, other health conditions, and symptoms.
- For women with a uterus: Estrogen is combined with progesterone to support uterine health. Women who’ve had a hysterectomy can use estrogen alone.
- Bioidentical hormone therapy: These match your body’s natural hormones, though they’re not automatically safer than traditional hormone therapy.
Nonhormonal treatments
Not everyone wants or can use hormones, and that’s totally fine. There are other options for symptom relief:
- Medications: Certain antidepressants (SSRIs, SNRIs) can help reduce hot flashes and also help support your mood. Gabapentin can help with hot flashes and sleep, while clonidine offers another option.
- Therapy: Cognitive behavioral therapy (CBT) tailored for menopause can help manage hot flashes, mood swings, and sleep challenges. It teaches you coping strategies and can have lasting benefits beyond treatment.
When to see a healthcare professional
Even though menopause is a natural phase, sometimes symptoms or changes signal that it’s time to get professional support. Knowing when to reach out helps you feel more in control and can make a big difference in your comfort and well-being.
- Hot flashes and night sweats: If these disrupt your daily life or sleep, don’t just grin and bear it. Medical treatments can make a real difference when lifestyle tweaks aren’t enough. Severe symptoms aren’t something you have to accept. They’re treatable.
- Irregular bleeding: Some fluctuation during perimenopause is normal, but certain patterns need a closer look. Bleeding after 12 months without periods, very heavy bleeding, or spotting between periods should be evaluated to rule out underlying conditions. Your doctor can help distinguish normal changes from something that needs attention.
- Mood changes: Feeling more anxious, sad, or irritable than usual is common, but if it starts interfering with work, relationships, or daily life, it’s worth getting help. Therapy, medication, or hormone management can all support mental health during this transition. Emotional well-being is just as important as physical health.
Reaching out for support isn’t a sign of weakness; it’s a proactive step in taking charge of this phase of life and finding ways to feel your best.
Embracing the next chapter
What is menopause? A challenging but empowering phase of your life! Understanding what menopause means can help you approach this transition with confidence and a little more ease.
Every woman’s menopause journey is unique. What works for a friend might not suit you—and that’s completely normal. Staying informed, talking openly with healthcare providers, and experimenting with approaches that fit your lifestyle helps you find what truly works.
Modern medicine offers more options than ever to help you feel comfortable and confident. Whether it’s hormone replacement therapy, lifestyle tweaks, non-hormonal treatments, or complementary approaches, there are solutions that can ease symptoms and improve quality of life. Wisp makes it simple with online menopause consultations, ongoing guidance, and discreet delivery of treatments right to your door.
Ready to take control of your menopause journey? Book a Wisp online menopause consultation today and get personalized support from the comfort of your couch.
This blog post is for informational and educational purposes only and should not be taken as professional advice. Always consult with a qualified professional before making any decisions based on the information provided here.